Diabetic Hypoglycemia

Diabetic hypoglycemia or low blood sugar, is very common in diabetics with type 1 diabetes and occurs occasionally in people with type 2 diabetes who are taking oral hypoglycemic drugs. Low blood sugar or hypoglycemia is usually the result of a mistake in insulin dose, exercise, and available carbohydrates usually due to a missed meal.
The symptoms of hypoglycemia or low blood sugar result from a compensatory autonomic nervous system reaction and from impaired cerebral function due to a significant decrease in glucose available for use by the brain. The onset of low blood sugar or hypoglycemia in diabetics is usually sudden with blood glucose levels of less than 45 to 60 mg/dL. In severe cases of hypoglycemia, death can occur.
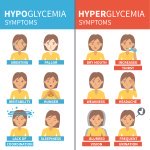
Hypoglycemia Symptoms
• Feeling very hungry
• Feeling Irritated
• Lightheadedness or dizziness
• Nervousness
• Confusion
• Slurring of speech
• Sweats
• Sudden change in personality
• Anxiety
• Sleepiness
• Weakness
The dangers of diabetic hypoglycemia:
Hypoglycemia or low blood sugar is especially dangerous if it occurs during sleep. The brain utilizes glucose exclusively for energy. And without adequate glucose, a diabetic may slip into a hypoglycemic coma. If this state is quickly reversed, by giving glucose, then no permanent damage occurs. However, if the low blood sugars levels persist for several hours, the nerve cells in the brain could begin to suffer some damages. This is where the damage to the brain may become more permanent.
This is why it is very vital that a person living with diabetes wears a medical alert bracelet letting people know they are diabetic.
Diabetics can experience two forms of Hypoglycemia; mild and severe
For mild hypoglycemia prompt treatment is necessary. Diabetics experiencing hypoglycemia or low blood sugar should take about 15g of a rapid-acting sugar. This amount of sugar is found, for instance, in three glucose tablets, three large marshmallows, five Life Savers candies, ½ cup of fruit juice or regular soda, 8 oz of skim milk, or 3 tablespoons of sugar or honey. Sugar should not be added to fruit juice in any situation. Adding sugar to the fruit sugar already present in the juice could cause a rapid rise in blood glucose, causing persistent hyperglycemia.
If for any reason the symptoms of hypoglycemia continue, the 15/15 rule should be followed. Wait for about 15 minutes, check blood sugar levels, and if it is still low, consumes another 15 grams of carbohydrate. This process can be repeated until blood sugar levels return to normal. Diabetics should try to have a source of carbohydrate readily available at all time so that they can quickly deal with hypoglycemic symptoms. If the hypoglycemia or low sugar level continues to happen for more than three times a week an adjustment of the diabetes management plan may be in order.
Diabetics who experience severe hypoglycemia or low sugar levels often need to be hospitalized to get their symptoms under control. The criteria for hospitalization are one or more of the following.
• Blood sugar level is less than 50 mg/dL, and the prompt treatment of hypoglycemia has not resulted in recovery.
• The diabetic has seizures, coma or altered behavior.
• The hypoglycemia has been treated; however, a responsible adult cannot be with the client for the following 12 hours.
• The hypoglycemia was as a result of a sulfonylurea drug.
Conclusion
Untreated, diabetic hypoglycemia can lead to loss of consciousness and seizure — a medical emergency. Rarely, it can be deadly. Tell friends and family what symptoms to look for and what to do in case you are not able to treat the condition yourself. It is also important to consult with your doctor in order to develop a management plan for situations like this.


New! Facebook Comments
What do you think? Share your thoughts below...